Having a baby is a wonderful time in your life, but the effects the pregnancy can leave on your body may be devastating. We all see how these celebrities lose all the weight and are wearing bikinis weeks after giving birth, and we think why can't that be me? Well, it takes a lot of work and dedication thats for sure!
Instructions
1 Each pregnancy is different and the amount of weight each person gains, and where she gains the weight vary from one to the next.
You want to make sure that you lose the weight a healthy and safe way. Otherwise you may gain it all right back. Crash dieting never works! You lose the weight and then it creeps back up on you, so beware of a quick fix! The best way to lose weight after a baby is the good old fashioned way...Diet and Exercise.
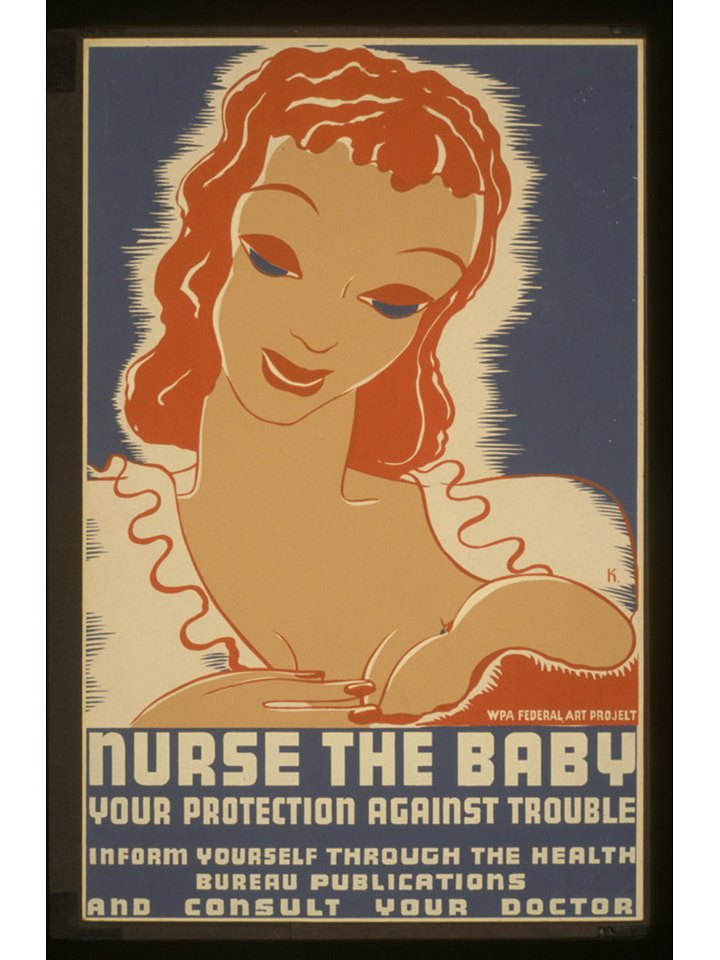
2 Of course you lose weight right away when the baby is born, and a certain amount of weight will normally naturally shed off as well. Breast feeding is a great way to speed up your weight lose as well. It is proven that breastfeeding sends out certain hormones to your body for the first 12 months after giving birth that help your uterus go back to its pre-pregnancy shape.
3 The average amount a woman gains during her pregnancy is between 25-35 pound. When she gives birth the normal amount that is often shed is 12 to 15 pounds. So that leaves the unwanted pounds to struggle with. Although this is just an estimated average for weight gain, that personally I was way over!
There are different programs that you can join for assistance such as Weight Watchers, Nutri-System, Jenny Craig, etc. These programs are helpful for moms that live a busy lifestyle and these days that pretty much includes us all!
4 The best way to lose the weight after baby is to stay healthy throughout your pregnancy in an ideal world! Eat healthy and get in plenty of activities to keep you active. Walking and other exercise that are safe when your are expecting. If you don't gain to much weight throughout your pregnancy there wont be much to lose after baby is here.
Your diet plays an important role in weight lose and weight gain. So here are some helpful tips to help with losing weight and eating healthy....
5 Here are some helpful tips to lose weight the safe way....
* Stop eating sugary foods. Just dropping the sugar from your diet can help you lose weight quickly. Make sure that you stay away from it all together if you want to lose weight quickly. This means no sugar in your coffee, on your cereals, or eating that candy bar!
* Cut the carbs from your diet. Carbohydrates turn into sugar inside our body's and makes you hold onto body weight and fat. Omitting carbs from your diet can help you drastically drop the unwanted pounds. These days there are many alternatives to diets without carbs that are tasty and nutritious.
6 * Increase fiber into your diet.
* Incorporate fruits and vegetables into your diet.
* Make sure you eat your dairy items. You can choose to have low fat or even fat free milks and yogurt's.
* Watch your portion sizes! Many people have no concept of the amount of food that hey should be eating. Here are some helpful tips about portion sizes...
3 ounces of meat, fish, chicken, etc. is about the size of the palm of a womans hand or a deck of playing cards.
An ounce of cheese is about the size of your thumb.
A teaspoon of butter is the about the size of your thumb tip.
Learning the correct portions that you should consume can greatly improve your weight lose.
7 * Stay aways from fried foods.
* Watch the calories. They count when you are trying to lose weight. Stick to a diet within a certain range of calories consumption ideal for you.
Of course you want to add exercise to your daily routine whenever possible. It may be difficult in the beginning since having a new baby is so much work, so take it easy and remember to not move it to fast. Listen to your doctors advice and do not overdo it! Take care of yourself and your baby and focus on the health of you guys before anything else!
8 The first year is a big change for you and for your baby, so manage where you can. Take it easy and simply watch what you put into your mouth. Stick to a healthy diet and exercise when you can. Incorporate baby activities that you can do to bond with baby while being active.
Don't stress yourself out about a few pounds here and there. Look at your little baby and see the miracle that your body created. So give yourself a break! You created that little miracle and it was all worth it!